Advanced Practice: Zebras in the ED
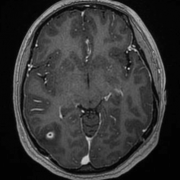
24 y/o F visiting from Guatemala with no medical history presented to the ER after a syncopal event from standing during which she fall backwards hitting her head on a hard surface. Patient was witnessed to be shaking while on the ground per family member. She continued to feel dizzy while in the ED. Her lab work was normal and a head CT was performed which showed the following:

Neurocysterosis
- CNS infection from the tapeworm Taenia solium
- Common in developing countries where it is the most common cause of secondary epilepsy
- Humans become infected by eating undercooked pork after which the parasite invades the brain parenchyma
- The developing larvae form cysts within the parenchyma leading to the inflammation and fibrosis seen above. Can cause hydrocephalus if they form in the ventricles.
- In the majority of cases, lesions (and thus seizures) resolve within 3-6 months. However, up to 20% of patients will have ongoing seizures and require antiepileptics
Diagnosis: Based on history, CT/MRI findings; serologic testing available but not required
Treatment: Antiepileptic monotherapy, antiparasitic agents (praziquantel and albendazole). Length of treatment varies based on number, location and viability of the parasites; therefore, treatment decisions should be made in consultation with infectious disease or neurology
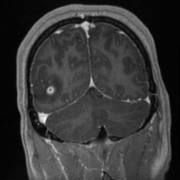
The patient in the above scenario was seen by neurology and infectious disease. She was started on keppra, two weeks of albendazole and a prednisone taper. Her MRI imaging is below:
References
- Blok, Barbara K., Cheung, Dickson S., Platts-Mills, Timothy F. First Aid for the Emergency Medicine Boards. 3rd ed. China. McGraw-Hill Education LLC, 2016. 844-845
- Stapczynski, J. Stephan,, and Judith E. Tintinalli. Tintinalli's Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York, N.Y.: McGraw-Hill Education LL
