Back to Basics: Swollen Joint
A Case of a Swollen, Painful Knee
By: Karen O'Brien, DO
The Case
A 64M with history of opioid use disorder (IVDU), HCV, HTN presented to the ED with left knee pain and swelling 10 days after mechanical fall onto that knee. He was unable to bear weight. His knee was extremely swollen with an effusion, warm, and he had severe pain with any ROM of the joint. His X-ray negative for fracture. What else could be causing this patient's swollen painful knee?
Particularly considering this patient's history of IVDU, septic arthritis was considered. The patient underwent an arthrocentesis with results below.
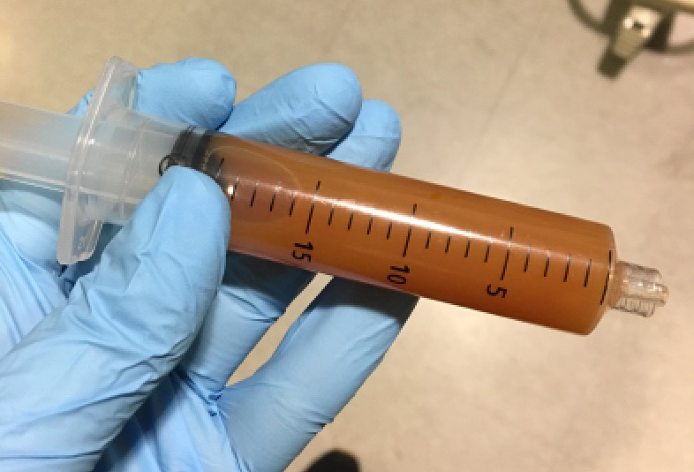
Aspirated 150cc cloudy fluid, cell count was 70K with 99% PMNs. Taken to OR for wash out for septic arthritis.
Septic arthritis:
- Acute hot swollen tender joint with decreased ROM (active and passive) is bacterial nongonococcal septic arthritis until proven otherwise!
- Frequently quoted joint fluid WBC >50K is not very sensitive, and ESR >30 is not very specific
- Management: admit even if arthrocentesis is nondiagnostic, IV abx (vanco and third gen cephalosporin such as CTX or cefepime), and consult ortho for possible washout
- Sickle cell? Salmonella! Give vanco and cipro!
- Suspect gonococcal if sexually active young adults; infection will typically have a prodromal phase of migratory arthritis and tenosynovitis before symptoms settle in one or more joints
- Joint fluid cultures are often negative! Culturing the posterior pharynx, urethra, cervix, or rectum increases the culture yield
- Rarely requires OR because less joint destruction than nongonococcal septic arthritis
- Predisposing factors: elderly, preexisting joint disease, recent instrumentation of that joint, skin or soft tissue infection, IVDU, indwelling catheters, immunosuppressed (including DM!)
Other D/dx:
- Osteoarthritis (OA)
- Rheumatoid arthritis (RA)
- Crystal-induced (gout vs pseudogout)
- Seronegative spondyloarthropathies such as ankylosing spondylitis
- Reactive arthritis (Reiter’s)
- Viral arthritis
The number of joints involved helps with differential
- 1 joint: nongonococcal septic arthritis (85% are monoarthritis but 15% are oligo including Lyme’s arthritis), gonococcal (also can be oligo), gout/pseudogout, traumatic arthritis, acute OA
- 2-3 joints (oligo): nongonococcal septic arthritis (especially Staph aureus and Strep pneumo), gonococcal arthritis, Lyme’s, reactive arthritis, rheumatic fever
- >3 (polyarthritis): RA, SLE, viral, chronic OA, serum sickness or serum sickness-like reactions
Labs:
- ESR and CRP are frequently elevated in acute inflammatory and reactive arthritides but not specific
- Obtain blood cultures
Imaging:
- Bedside US is helpful for identifying an effusion and aids in successful joint aspiration
- Obtain XR if suspect trauma or osteomyelitis
Reference:
Burton JH, Fortuna TJ. "Joints and Bursae." Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e. Judith E. Tintinalli, et al. New York, NY: McGraw-Hill, 2016.
