Board Review: Lets get cerebral
A 25-year-old female presents to the ED with generalized weakness associated with diplopia noticeably worse at the end of her work day for the past few days. Initially she attributed these symptoms to stress at work especially given that her symptoms improve with rest. On exam you notice significant ptosis bilaterally and speech is mildly slurred. She denies any numbness. What is the best option below to determine whether this patient is at higher risk for impending respiratory failure?
A. FVC
B. SpO2
C. PaCO2
D. Respiratory Rate
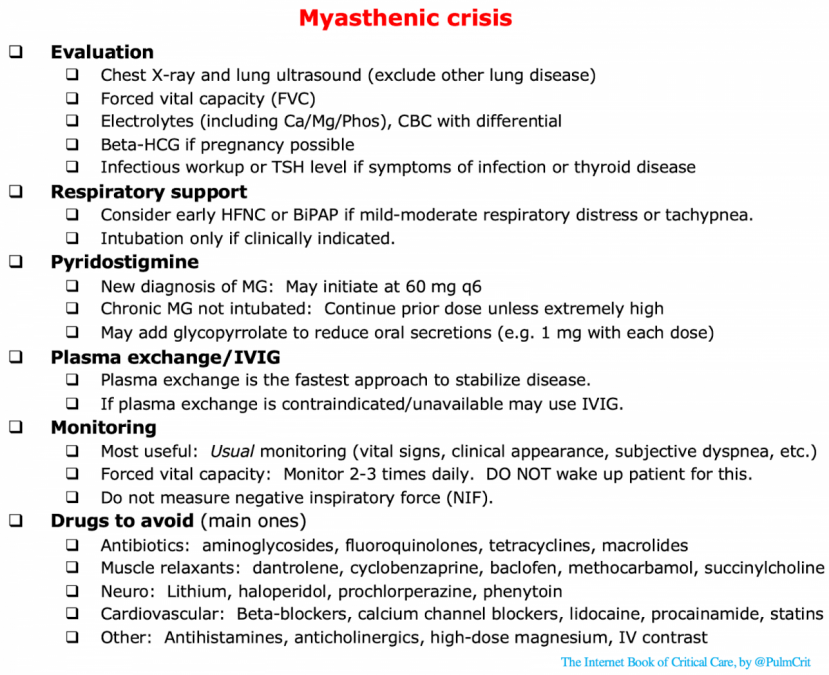
A. FVC. This patient has symptoms of myasthenia gravis, a diagnosis manifested by skeletal muscle fatigability caused by acetylcholine receptor antibodies at the neuromuscular junction. Myasthenic crisis is the main concern at this ED visit as she has signs of bulbar involvement indicating possible impending respiratory failure. Keep in mind that accessory muscle use may not be present in the patient with significant muscle weakness, so this patient may not appear to be in distress at first. FVC (Forced Vital Capacity), the largest volume a patient can exhale, reflects inspiratory and expiratory strength. An FVC <20-30 ml/kg indicates a need for ICU-level monitoring for respiratory failure. NIF (Negative Inspiratory Force) has also been used however is more effort-dependent and less reproducible. The decision to intubate a patient, however, should be made based on your overall clinical assessment of the patient at the bedside.
See this prior EM daily post about intubating patients with myasthenia gravis: https://emdaily.cooperhealth.org/content/advanced-practice-pearls-myasthenia-gravis-intubations
