Critical Cases - Post LP Subdural Hematoma!
Tue, 07/20/2021 - 5:11am
Editor:
HPI
- 24 yo female hx of gradual onset severe frontal/bitemporal HA for 4 days, no history of similar
- Unresponsive to acetaminophen
- Worse lying down, better sitting up
- Associated with intermittent blurred vision and subjective loss of balance while walking
PE
- VS: T 97.9 HR 63 BP 113/70 Pox 100% on RA
- Looks in no distress
- PERRL, EOMI, visual acuity: OD 25/20 OS 25/20
- Neck is supple
- Neuro: alert and conversant. Ambulates with steady gait. 5/5 strength in UE/LE b/l, neg pronator drift. Normal finger to nose
DDx
- Primary HA: the most common headache encountered in the ED, includes: tension, migraine, cluster
- Subarachnoid hemorrhage: no abrupt onset however a "severe and unusual" headache
- Cerebral venous thrombosis: Pt is obese, but not on OCP, not postpartum, and no hx of coagulopathy
- Meningitis: Possible, but no fever and neck is supple. HA for more than 2 days is highly unlikely to be acute bacterial meningitis in a well appearing, afebrile patient
- IIH: Actually more common than ruptured subarachnoid hemorrhage, usual presentation is just moderate/severe, unusual headache. Is associated with OCP use, Vitamin A use, and tetracycline use
Workup
- Noncontrast CT: negative
- urine pregnancy: negative
- Lumbar puncture performed: Opening pressure = 26 cm H20, no xanthochromia, cell counts WNL
- CSF drained 17 ml clear fluid, closing pressure = 19 cm H20
- A CT venogram is performed to rule out cerebral venous thrombosis (mandatory to exlude in possible cases of IIH) which is negative
- Pt feels better and is dc'd home on oral acetazolamide with instructions to follow up with neurology and opthalmology
Return visit
- Pt returns 2 days later with worsening of her initial headache
- Her neuro exam is unchanged
- A repeat lumbar puncture is performed with an opening pressure of 8 cm H20 and closing pressure of 3 cm H20
- Pt HA fails to remit, prompting admission with neurology consult
- An MRI of the brain is subsequently ordered which shows:
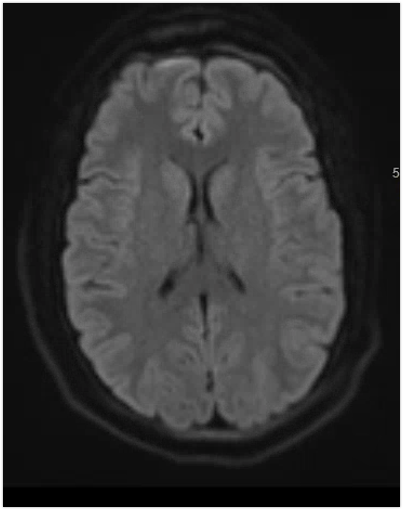
- MRI brain: "multifocal small acute subdural hematoma" (best seen here adjacent to R frontal lobe)
Outcome
- Pt underwent serial CT scans and did not require neurosurgical intervention
- Discharged home in good condition
Discussion
- This patient sustained subdural hematomas as a complication of serial lumbar punctures, which decreased the intracranial pressure to the point that the brain "sagged" down and pulled away from the skull, resulting in small tears to the briding veins to the skull
- This a rare but important potential complication of an LP and should be considered in all post-LP headaches who present with any neurological symptoms other than headache
- A noncontrast CT should detect the majority of post-LP subdural hematomas
- Management is similar to traumatic subdural hematomas
