#EMConf: Head Injuries
Thu, 02/25/2021 - 5:00am
Editor:
General Terminology:
- Traumatic Brain Injury: Brain function impairment that results from external force
- Glasgow Coma Scale: Says nothing about underlying structural brain injury, but provides a common language across consultants and is effective for measuring recovery and response over time
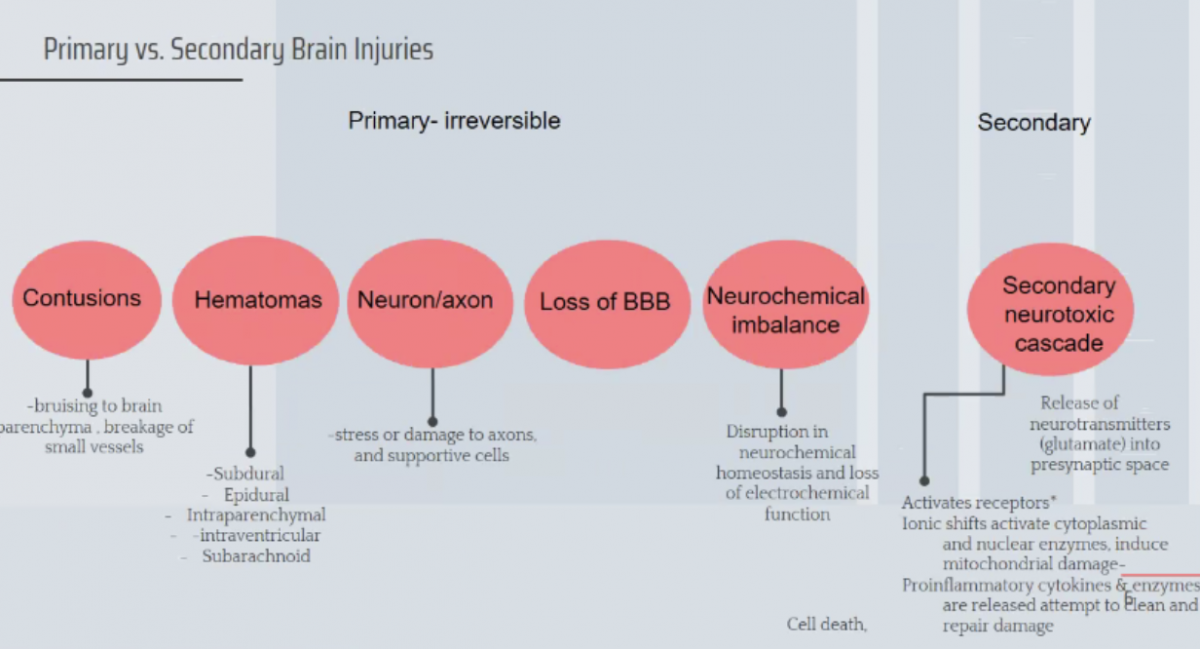
- Primary vs secondary brain injuries:
Classification of TBI
- Mild (GCS 14-15) = 80% of TBIs; can be a concussion, but can lead to significant debilitating long term sequelae
- Moderate (GCS 9-13) = 10% of TBIs; 20% mortality for isolated injury, but only 40% will have an abnormal CT finding
- Severe TBI (GCS 3-8) = 40% mortality, often in the first 48 hours; <10% have good neurologic recovery
Goals for Management of Elevated ICP Secondary to Traumatic Brain Injury: Prevent Secondary Injury!
- Elevate HOB 30 degrees to decrease ICP and improve oxygenation
- PaCO2 is the most powerful determinant of cerebral blood flow, with a goal of 35-45 mmHg (NORMAL)
- Goal PaO2 >60mmHg with SpO2 >90%, basically avoiding hypoxia
- Also want to avoid hypotension (GOAL CPP >60mmHg; CPP = MAP-ICP so you want MAP 100-110)
Management of Elevated ICP Secondary to Head Bleed
- Head CT (sometimes serial imaging)
- Early neurosurgery consult
- Bolt” = EVD / Ventriculostomy/ parenchymal pressure monitor to directly measure ICP
- Emergent Decompressive Craniectomy: Removal of a portion of the skull to allow for brain edema and to avoid downward herniation
- Reverse anticoagulation
- Heparin: Protamine
- Warfarin: PCC or FFP or IV vitamin K
- DOACs: PCC; for particular DOACs = Idarucizumab for Dabigatran, Andexanet Alfa for Xa inhibitors (Rivaroxaban and Apixaban)
- ASA or Clopidogrel: Platelet transfusion
- Consider seizure prophylaxis
- Mannitol or Hypertonic saline
Patterns of Hematomas
- Epidural: Direct blow to head, usually at pterion, injury to middle meningeal artery
- Brisk bleeding
- Initial LOC then lucid interval, then neuro deterioration
- Need urgent neurosurg consult and possible intervention
- Lens shaped bleed does not cross suture line
- Subdural: Elderly, sudden acceleration-deceleration injury
- Tearing of bridging veins, SLOW venous ooze, therefore may not be symptomatic until days or weeks after initial injury
- Elderly or alcoholic
- Crescent shaped, crosses suture lines
- Acute bleed = < 2 weeks vs chronic bleed >2 weeks
- Usually these do not require surgical intervention; greater mortality if they do
- Traumatic SAH: Sudden deceleration injury causing shearing of blood vessels into the subarachnoid space
- Most common CT abnormality in moderate to severe TBI
- Most sensitive is CT 6-8 hours AFTER injury, can be missed on early CT
- Rebleeding is very common
- Large traumatic SAH may dissect into the ventricles, causing hydrocephalus
- Traumatic SAH blood tends to collect on the brain periphery (in the cerebral sulci) vs. spontaneous SAH causes central collection of blood in the basal cisterns (star pattern)
- Cerebral Hematomas/Contusions: Deceleration injury, severe trauma, penetrating trauma, shaken baby syndrome
- Collections of blood WITHIN the brain parenchyma and along the base of the brain (irregular contour)
- Most commonly= frontal and temporal
- White lesions with surround edema (darker) that expand overtime and can result in mass effect and herniation
- No real surgical management; just do serial CTs
DAI = Diffuse Axonal Injury:
- Occurs as a result of traumatic deceleration
- Shearing of AXONS in the deep white matter
- Typical clinical picture: Comatose patient with no or minimal signs of injury on initial head CT; MRI shows extent of the damage!
- Devastating prognosis, can progress to massive swelling and herniation within hours or days after injury
- Treatment is supportive
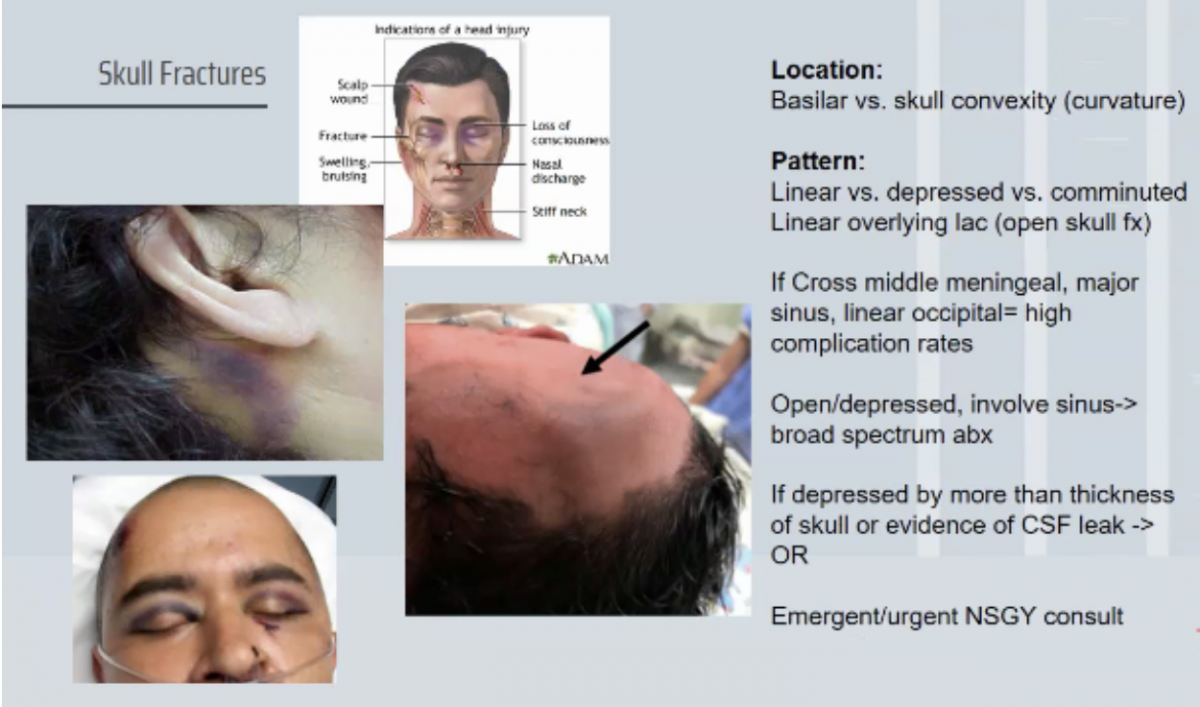
Skull Fractures: