#EMConf: Tuberculosis
Thu, 11/19/2020 - 7:43am
Editor:
General:
- TB throughout history was known as the “consumption” or the white plague and there is evidence that TB may have existed even 500,000 years ago. Despite this, it was only in the last century that the first treatment, streptomycin, was developed.
Epidemiology:
- TB is one of the leading causes of death around the world
- Every year 10 million people become infected with the disease and 1.5 million people die
- In the US, the highest incidence is among foreign born individuals
Pathophysiology:
- TB is caused by mycobacterium tuberculosis, an intracellular bacterium that is transmitted via droplet and aerosolization
- Infection can be primary, latent, or post-primary/ reactivation disease
Clinical symptoms:
- During primary TB infection, patients can present subclinically or like community acquired pneumonia.
- Latent TB can present asymptomatically, but patient will have a positive PPD test
- Active TB disease (often reactivation disease) can present with fevers, chills, weight loss, night sweats, and hemoptysis
- Occasionally, younger patients or people who are immunocompromised can present with extrapulmonary disease
Management:
- Suspect TB in patients with HIV complaining of cough, foreign born patients with symptoms suggestive of TB, and patients with exposure.
- Place a mask on the patient and order respiratory isolation precautions
- Wear N95 and proper PPE
- Order a chest x-ray
- The diagnosis will not be made in the ED, but keep it on the differential in select patients
- Do not start antibiotic treatment in the ED without consultation with the infectious disease specialists
Imaging:
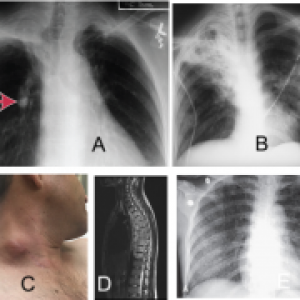
- Primary TB can present with a tuberculoma, formed in response to the bacteria (A)
- Post primary TB can present with upper lobe cavitary disease (B)
- Cervical adenopathy is called scrofula (C).
- Potts disease-TB of the thoracic spine (D)
- Miliary TB-seen when the host cannot contain the infection (E)
Disposition:
- Consider admission for patients that are immunocompromised or have active TB
- Patients with latent TB or healthy individuals with suspected TB can be discharged after consultation with local health officials
References:
- Cavalhiero A, Shin S, Seung K, Furin J. Tuberculosis. In: Ryan E, ed. Hunter's Tropical Medicine And Emerging Infectious Diseases. 10th ed. Elsevier; 2020.
- Long B, Koyfman A. Tuberculosis. In: Tintinalli JE, Ma O, Yealy DM, Meckler GD, Stapczynski J, Cline DM, Thomas SH. eds. Tintinalli's Emergency Medicine: A Comprehensive Study Guide, 9e. McGraw-Hill; Accessed October 27, 2020.
- Pacifique M, Alcala C, Bryant SM. Cervical Tuberculosis Lymphadenitis. Visual Diagnosis in Emergency Medicine 2018. 54(6) E141-142.
- Sokolove P, Derlet R. Tuberculosis. In: Walls R, ed. Rosen's Emergency Medicine: Concepts And Clinical Practice. 9th ed. Philadelphia; 2018.
- https://radiopaedia.org/articles/tuberculosis-pulmonary-manifestations-1...
