Jaw Dislocation
Temporomandibular Joint (TMJ) Dislocation
AKA Jaw Dislocation
AKA "Doc I can't close my mouth"
Background
- Most commonly atraumatic
- Extreme opening of the mouth - yawning, eating, laughing, singing, dental treatment, etc.
- Can result from dystonic reactions secondary to drugs, seizure, tetanus infection
- Most commonly anterior
- Posterior and superior dislocation typically occur only in high-energy trauma, rare
- Superior: think mandibular fossa fracture
- Posterior: think temporal plate fracture or disruption of external auditory canal
- Most commonly bilateral
- Often recurrent
- Risk factors: patients with an anatomic mismatch between fossa and articular eminence, weakness of capsule and TMJ ligaments (ie Ehlers-Danlos, Marfans), torn ligaments, prior dislocation
- Diagnosis: Made clinically if atraumatic; CT or panoramic x-ray is indicated in cases of trauma
- Treatment: Closed reduction
Reduction Techniques
Syringe Technique:
- Place a 5 or 10 mL syringe between the upper and lower posterior molars on one of the affected side
- Instruct the patient to bite down gently while rolling the syringe back and forth between the teeth until that side is reduced
- Typically, opposite side will then reduce spontaneously
- High success rate with cooperative patients

Gag Reflex Technique
- In an awake patient, use a tongue depressor to stimulate the posterior soft palate
- Causes muscle relaxation, mandible descends caudally so that the condyle moves inferiorly and relocates into place
Intraoral Techniques:
- Several maneuvers beginning with physician’s hands in patient’s mouth
- Provider must wrap fingers in gauze prior to maneuver to prevent being bitten by patient; also consider taping shorted tongue blades to thumbs and/or placing bite block
- Techniques are typically done with patient sitting upright with an assistant holding the head still, although one can consider positioning patient supine
- Classic:
- Place thumbs on posterior lower molars while using other fingers to wrap around mandible externally
- Apply steady downward pressure to free the condyles from the anterior aspect of the eminence, then guide then guide the mandible posteriorly and superiorly back into the fossa

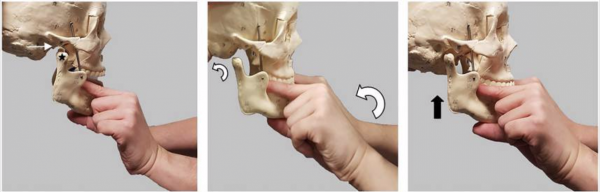
- Wrist Pivot:
- Place thumbs externally under the chin with fingers on the posterior lower molars
- Apply steady upward pressure with the thumbs with simultaneous downward pressure to the lower molars
- Then pivot both wrists forward - this should result in successful bilateral reduction
- Be sure to apply steady pressure equally to all sites to avoid mandibular fracture
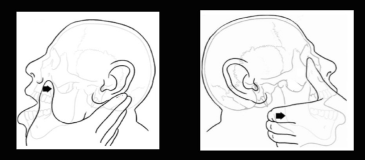
Extraoral Technique:
- Technique reduces one side of a bilateral TMJ dislocation; the second side then typically reduces spontaneously (or maneuver can be repeated on opposite side)
- Physician places fingers externally over mandibular angle on one side with thumb over malar eminence of the maxilla
- On opposite side, palpate the dislocated coronoid process with thumb while placing finger behind the mastoid process
- Simultaneously apply forward pressure to the mandible while pushing the coronoid process backward with opposite hand
Post reduction:
- Reduction can be confirmed clinically if jaw feels back in place, dental occlusion is normal and patient is not having significant pain with jaw movement
- If there is concern for iatrogenic fracture or unsuccessful reduction, consider panoramic jaw x-ray
- Apply self-adherent wrap or kling wrap around head supporting jaw while recovering from sedation
- Instruct patient to avoid extreme jaw opening for 3 weeks, support lower jaw while yawning
- Maintain soft diet for 1 week
- NSAIDs and warm compresses for pain
- Discharge with OMFS follow-up in 2-3 days
References:
Mendez D.R. et al. Reduction of temporomandibular joint (TMJ) dislocations. In: UpToDate, Post TW (Ed), UpToDate, Waltham, MA.
Roberts, J. R., In Custalow, C. B., In Thomsen, T. W., & In Hedges, J. R. (2014). Roberts and Hedges' clinical procedures in emergency medicine.
Tintinalli J.E., & Stapczynski J, & Ma O, & Yealy D.M., & Meckler G.D., & Cline D.M.(Eds.), (2016). Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e. McGraw-Hill.
Gorchynski J, Karabidian E, Sanchez M. The "syringe" technique: a hands-free approach for the reduction of acute nontraumatic temporomandibular dislocations in the emergency department. J Emerg Med. 2014 Dec;47(6):676-81. doi: 10.1016/j.jemermed.2014.06.050. Epub 2014 Sep 30. PMID: 25278137.
