Pediatric Epileptic Syndromes
Thu, 04/22/2021 - 5:00am
Editor:
Etiology of Seizures & Epilepsy:
- Infants, Children: Prenatal or Birth injury vs. Inborn Errors of Metabolism vs. Congenital Malformation
- Children, Adolescents: Idiopatchi or Genetic vs. CNS Infection vs. Trauma
- Adolescents, Young Adult: Head Trauma vs. Drug Intoxication or Withdrawal
Seizure Type: determed by patient's behavior and EEG pattern during the event
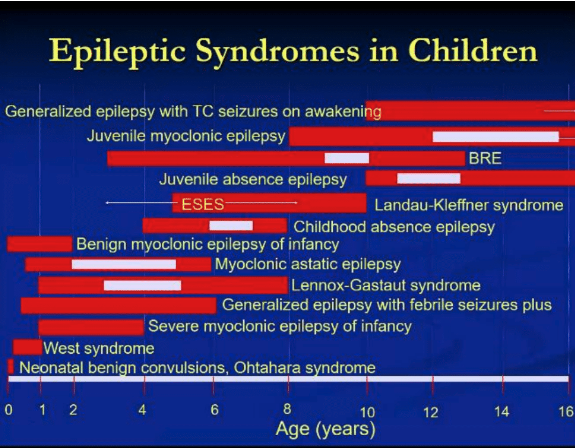
Epilepsy Syndrome: defined by age at onset, seizure types, EEG patterns and family history
Case 1:
- HPI: 5 month old with no past medical history presents with concerns for jerking movements of head and arms
- Exam: healthy child, mild truncal hypotonia
- EEG: Hypsarrhythmias
- Diagnosis: West Syndrome (Infantile Spasms)
- Sudden, symmetric, tonic muscle contraction production flexion/extension of truck and extremities
Case 2:
- HPI: 4 year old history of birth related HIE and resultant static encephalopathy presents with episodes of head drops & staring spells & occasional falls
- Exam: Microcephaly, cognitive delays, spasticity
- EEG: shows diffuse 2-2.5 Hz spike wave (slow spike & wave activity)
- Diagnosis: Lennox-Gastaut Syndrome
- Frequent seizures, mental retardation, resistance to drug therapy, mixed seizure disorder (atonic, tonic, atypical absence)
- Onset peaks at 3-5 years of age
Case 3:
- HPI: 9 year old presents with first time seizure. Nocturnal, speech arrest, drooling followed by left face and arm clonic activity
- Exam: non-focal & normal development
- EEG: EKG like morphology of waves with this type of epilpesy (sharp spike & slow wave); normal back ground with centrotemporal spokes activated by drowsiness and sleep ipsilateral to side of body with clonic activity
- Diagnosis: Benign Rolandic Epilepsy
- Age of onset is late childhoold (~3-10 years of age)
- Low frequency of seizures thus don't treat the first seizure!
- 25% of patients have 1 seizure; 50% of patients have < 5 seizures
- Epilepsy usually remits by 16 years of age
- Speech involved & if occurs upon waking up at night, think Benign Rolandic Epilepsy
- Seizure Type: simple partial motor in ~75%, involving face, oropharyngeal muscles and upper limb with retained conciousness
- Some patients have Learning Disabilities
- Management: unclear if truly necessary but patients get a good repsonse with Carbamazepine & Oxcarbamazepine
Case 4:
- HPI: 6 year old with declining school performance, staring spells. Normal birth history and development
- Exam: normal
- EEG: bursts of 2.5 to 3.5 Hz spike and wave induced by hyperventilation with brief unresponsiveness; normal background
- Diagnosis: Absence Epilepsy
- Occurs around age 4 to 8 years old but can also start during puberty
- More common in females
- Simple: brief, staring episodes, unresponsive, motor arrest
- Complex: oral or motor automatisms, autonomic phenomenom, incontinence
- abrupt onset and offset, NO POSTICTAL STATE, which is how you differentiate from complex partial seizures
- Management: Ethosuximide or Valproate
Case 5:
- HPI: 15 year old healthy teenager with first "grand mal" seizure occured in setting of sleep deprivation. Sometimes "clumsy" in the morning, drops things, sometimes jerks after awakening.
- Exam: normal along with normal labs and MRI
- Diagnosis: Juvenile Myoclonic Epilepsy
- Precipitated by fatigue, alcohol, sleep deprivation; 40% have a family history
- Seizures recur in 80-90%; minority have seizure remission
Epilepsy Mimics:
- Syncope
- Metabolic Derangements
- Migraine
- Cerebral Vascular Disorders
- Sleep Disorders
- GI Disorders
- Psychiatric Disorders (such as PNES)
- Respiratory Conditions
