Vasopressors & Ionotrope Review
Fri, 04/16/2021 - 7:00am
Author:
Editor:
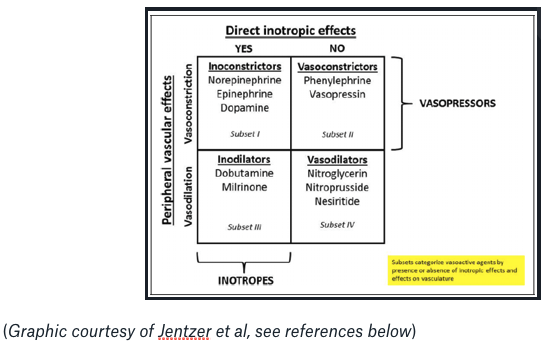
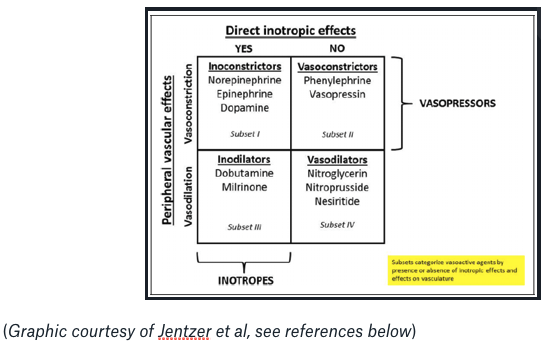
“Vasopressors” {V} restore MAP by increasing SVR via arteriolar vasoconstriction.
[We use vasoconstrictors to increase BP.]
“Ionotropes” {I} increase CO and SV via improved cardiac contractility.
[We use both ionoconstrictorsand ionodilators to increase BP.]
See below for a *brief* review of the main vasopressors & inotropes we use on the critical care side of emergency medicine!
{V}{I} Levophed(Norepinephrine):
- First line for most shock states - to supplement fluid resuscitation(if needed) in hypovolemic shock; for septic shock; for cardiogenic shock.
- Dosing: 0.05 mcg/kg/min, max of 0.2 mcg/kg/min(generally up to 40mcg/min, though no true‘cap’)
- Safe to give through PIV up to 10mcg/min(some might argue up to 20…)
- Theoretical risk of decreasing CO in patients w/ cardiac dysfunction(due to increase in afterload); however, most are able to maintain CO while on NE.
{V}{I} Epinephrine:
- Increases SVR & CO. Potent ionotrope, but also acts as a vasoconstrictor particularly with higher doses.
- Dosing: 0.02-0.05ug/kg/min
- Most useful for hypotensive patients w/o myocardial ischemia, especially after cardiac surgery, as well as a second line agent for patients in septic shock already on NE.
{V} Phenylephrine:
- Acts as a pure alpha1 agonist, ie no ionotropic effects. Increases arterial & venous tone.
- Dosing: 40-180mcg/min(avoid high end of dosing to prevent tissue ischemia)
- Often utilized for neurogenic shock(hypotension is thought to be 2/2 vasodilation), or less often septic shock if NE triggered an arrhythmia and/or in the setting of persistent hypotension with high cardiac output.
{V} Vasopressin:
- Increases SVR, decreases CO. No inotropic effects.
- Dosing: start at 0.01units/minute, up to 0.03 units/minute
- Typically used as a second line agent for patients with low SVR and/or tachyarrhythmias 2/2 NE treatment. No evidence to suggest that vasopressin should be given to help replete catecholamine deficiency in shock patients.
{V}{I} Dopamine:
- Effects are strongly dose dependent.
- low dose(0.5-2mcg/kg/min) - inodilation
- high dose(>10mcg/kg/min) - inoconstriction(progressively increase SVR without increasing CO)
- Used to be recommended for septic shock, but no longer is.
- Sometimes still used for septic patients with relative bradycardia with low risk for tachyarrhythmias.
{I} Dobutamine:
- Decreases SVR, increases CO.
- Dosing: start at 5 mcg/kg/min, increase in 2.5 mcg/kg/min increments to max of 20 mcg/kg/min
- Preferred over milrinone for patients with septic shock with myocardial dysfunction, cardiogenic shock, & renal failure patients.
- Can be used in combination with dopamine; studies have shown improved effects by utilizing both at lower doses compared to utilizing either at a higher dose.
{I} Milrinone:
- PDE receptor agonist(cAMP target)
- Decreases SVR(& pulmonary vascular resistance ie PVR), increases CO.
- Dosing: 50 mcg/kg loading dose followed by 0.375-0.75 mcg/kg/min(dose adjustment needed for renal dysfunction)
- Preferred over dobutamine in patients with RV dysfunction 2/2 reduction of PVR.
- Suboptimal for many patients with shock because those with hypovolemia(ie low SVR) may become more hypotensive after milrinone administration. Avoid using with renal failure 2/2 risk of drug accumulation.
{V} Midodrine:
- The only“PO” vasopressor. Alpha 1 agonist(ie, youcan sort ofthink of it like an oral version of phenylephrine).
- Dosing: typically start at 10mg q8h, with escalation to 15-20mg q8h if needed
- More so used for the outpatient treatment of orthostatic hypotension, as well as in combination with octreotide for the treatment of hepatorenal syndrome.
- Dosing regimen needs to be adjusted in chronic renal failure patients.
{V} Methylene blue:
- Non-adrenergic vasopressor.
- Dosing: 1-2mg/kg as a single dose, to re-dose if necessary
- Study showed that combination of hydroxocobalamin & methylene blue may be associated with decreased vasopressor requirement than methylene blue alone(Feih et al.)
- Typically used for shock refractory to other vasopressors, as well as for vasoplegia patients on cardiopulmonary bypass.
- Risk of serotonin syndrome as a side effect. Contraindicated in G6PD deficiency & ARDS.
Final tips/tricks:
- Always remember… MAP = CO x SVR !
- Refractory shock? Think about using methylene blue… but also always think of adrenal insufficiency!(Ie, discuss with your critical care colleagues / consider starting high dose steroids)
- Refractory anaphylactic shock? If multiple rounds of epinephrine are not effective, consider glucagon(especially if patient has HTN / is on a B blocker) +/- atropine!
- Remember that for obstructive shock, if a component is 2/2 HOCM/LVOT, consider adding esmolol to maintain a lower HR(high HR can worsen the obstruction).
References:
