What's the diagnosis? By Dr. Becca Fieles
A 65 yo male with a history of ESRD/HD, DM, HTN, CAD, PAD presents with abdominal pain. Pt reports he was weak and dizzy while on hemodialysis yesterday when his blood pressure dropped. He received some IV fluids and symptoms improved. He subsequently developed right sided abdominal pain that became severe. A CT is shown. What's the diagnosis? Scroll down for answer.

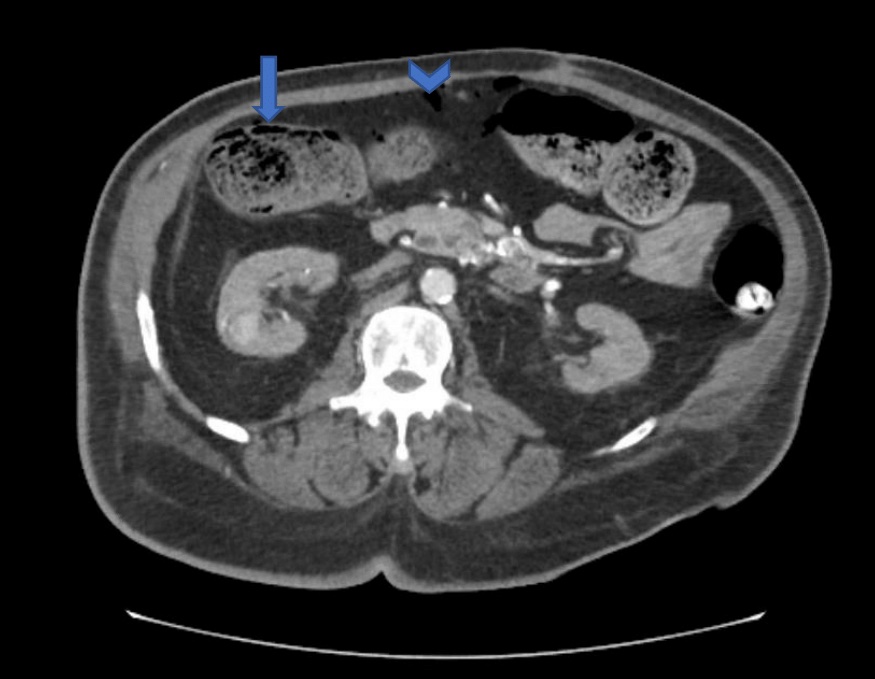
Answer: Ischemic colitis with pneumatosis and bowel perforation
long arrow showing pneumatosis coli (air in the wall of the intestine)
short arrow showing pneumoperitoneum (free air in the abdomen)
Etiology - reduction in mesenteric blood flow leading to ischemia
- occlusive disease - thrombus/embolus, small vessel disease, atherosclerosis, diabetes vasculitis, hypercoagulable state, sickle cell, aortoiliac reconstruction
- non-occlusive disease - CHF, shock states, hemodialysis, hypovolemia, diuretics, cocaine, volvulus
Presentation
- acute onset abdominal cramping and pain
- may develop hematochezia within 24 hours
- diarrhea, abdominal distention, nausea/vomiting
- classically 'pain out of proportion to clinical exam,' but may develop peritoneal signs with more advanced disease / full thickness necrosis
- progresses to sepsis, shock
Differential diagnosis - diverticulitis, colon ca, IBD, infectious colitis, peptic ulcer disease, AAA, SBO, pancreatitis, cholecystitis
Labs and imaging
- leukocytosis, lactic acidosis
- xrays are rarely helpful unless perforation leads to obvious free air in abdomen
- CT scan
- non-gangrenous disease - bowel wall thickening, thumbprinting, pericolonic stranding +/-ascites
- gangrenous disease may show pneumatosis coli, pneumoperitoneum
- submucosal edema or hemorrhage following reperfusion
Management
- non-severe disease (without peritoneal signs, no perforation)
- optimize reperfusion with IV fluids, optimized cardiac output, oxygen as needed, bowel rest, broad spectrum antibiotics due to disruption of mucosal barrier potentially leading to bacterial translocation
- severe disease (peritoneal or perforation)
- surgical management - bowel resection
Reference
Washington C, Carmichael JC. Management of ischemic colitis. Clin Colon Rectal Surg.2012;25(4):228-235. doi:10.1055/s-0032-1329534
