APRV to the rescue
APRV Basics
Airway pressure release ventilation (APRV) is a mode that helps with alveolar recruitment and stability by maintaining an open lung. The breath type delivered in APRV is time-triggered, pressure-limited and time-cycled. The pressure level alternates between the plateau pressure (Phigh or CPAP phase) and a low pressure setting (Plow). Most of the respiratory cycle is spent at Phigh, so the duration of time at Phigh (termed Thigh) significantly exceeds that of Tlow. The goal of APRV is to slowly open and recruit atelectatic or fluid-filled alveoli. The pressure release phase to Plow is short (Tlow) to enable ventilation and CO2 removal, while preventin derecruitment. In the absence of neuromuscular blockade, APRV allows for spontaneous breathing at Phigh. Theoretically, spontaneous breathing on APRV can increase aeration in the dependent lung, making ventilation more homogenous, augmenting V/Q matching and reducing dead space.
APRV is a unique mode where auto-PEEP (or intrinsic PEEP) is actually desired to provide positive end-expiratory pressure and avoid de-recruitment and atelectrauma. The Tlow must be set sufficiently short to ensure adequate intrinsic PEEP. Auto-PEEP can be quantified with an end-expiratory hold maneuever. The time-controlled adaptive ventilation (TCAV) protocol is a method of adjusting Tlow to terminate the release phase at 75 percent of peak expiratory flow. This prevents full exhalation and ensuing atelectrauma. As a patient’s lung compliance improves, the slope of the expiratory flow curve decreases (the lung deflates more slowly), and Tlow can be increased to maintain termination of expiratory flow at 75 percent of peak (Figure 1).
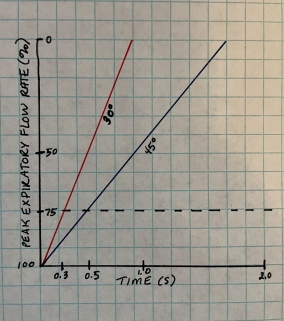
Figure 1. Expiratory flow curve of a patient with poor lung compliance (red) with a steep expiratory flow curve (30 degrees) requiring a shorter release time (0.3 seconds). As the lung recruits, the compliance improves (blue) and the slope of the expiratory flow decreases to 45 degrees.
What patients are candidates for APRV?
Patients with acute lung injury, ARDS, severe atelectasis, and multifocal pneumonia may benefit from APRV given the reduced lung compliance and alveolar collapse or flooding leading to V/Q mismatching.
Does APRV help patients get off the ventilator sooner?
In 2019, Carsetti et al. performed a meta-analysis of randomized controlled trials that sought to answer whether patients with acute hypoxemic respiratory failure with a PaO2/FiO2 ratio < 300 mm Hg treated with APRV had more ventilator-free days at day 28 compared to those treated with conventional ventilation strategies. Their final analysis included 5 single-center RCTs with a total of 313 patients. Ventilator-free days were lower in the APRV group, with an overall mean difference (MD) of 6.04 days (95%CI 2.12, 9.96, p = 0.003). Patients treated with APRV had a lower ICU length of stay than patients treated with conventional ventilation, with MD of 3.94 days (95%CI 1.44, 6.45, p = 0.002). The use of APRV was also associated with lower hospital mortality. It was noted by the authors that the studies included were lower quality, not blinded, and had a moderate amount of heterogeneity for the primary outcome. Their results should be interpreted with caution, as more RCTs need to be conducted to confirm their findings. To read the full study, click here.
Thoughts to consider in APRV
Although APRV has many benefits, it is important to note that spontaneous breathing could contribute to ventilator-induced lung injury, if patient effort increases transpulmonary pressure to an unsafe level. Additionally, tidal volume in APRV is a dependent variable, and may exceed lung protective settings, depending on the compliance of the lung, patient effort, airway resistance and pressure and time settings.
References:
Carsetti, A., Damiani, E., Domizi, R. et al. Airway pressure release ventilation during acute hypoxemic respiratory failure: a systematic review and meta-analysis of randomized controlled trials. Ann. Intensive Care 9, 44 (2019).
Kollishch-Singule M, et al. The time-controlled adaptive ventilation protocol: mechanistic approach to reducing ventilator-induced lung injury. Euro Respir Rev 28 (2019).
