The basics of Airway Pressure Release Ventilation (APRV)
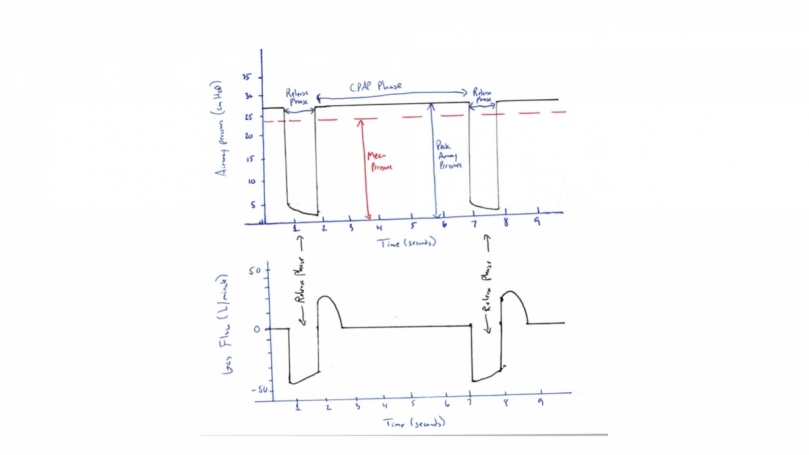
If you have been paying attention to the critical care literature in the era of COVID-19, you may have heard some mechanical ventilation strategies that are new to you. Airway Pressure Release Ventilation (APRV) is most often utilized as salvage therapy refractory acute respiratory distress syndrome (ARDS). ARDS is an acute diffuse, inflammatory lung injury leading to capillary leak and loss of aerated lung tissue. The pathophysiology of ARDS is characterized by alveoli that are collapsed or filled with protein-rich fluid resulting in perfusion with little to no ventilation (i.e. low V/Q or high shunt fraction). APRV delivers a time-triggered, pressure-targeted and time-cycled breath that resembles continuous positive airway pressure (CPAP) with periodic release from a high pressure (P high) to a low pressure (P low). APRV is not a new concept and was first described in the literature in 1987. The goal of ventilating a patient with APRV is to recruit and reopen collapsed alveoli to enable participation in gas exchange. By prolonging inspiratory time at P high and minimizing time at P low (end-expiratory pressure), V/Q matching is maximized. The time at P low is brief to ensure that end-expiratory pressure never reaches zero, producing intrinsic PEEP that prevents derecruitment during expiration. APRV can be conceptualized as CPAP with intermittent release and allowance for spontaneous breathing throughout the respiratory cycle. Below is a simplified breakdown of the ventilator settings, pressure-time and flow-time waveforms. Keep in mind, there are different strategies for setting, monitoring, troubleshooting, and weaning APRV, which requires considerable training. This review is only meant to act as a mental model to understand the basic concepts.
There are 5 key parameters to set in APRV:
- P high: P high can be considered the target plateau pressure. P high determines the mean airway pressure and the driving pressure of the released breath, depending on the degree of intrinsic PEEP. P high is typically set between 20 and 35 cm H20. Excessive P high can lead to alveolar overdistention and impair hemodynamics. If P high is too low, the patient may suffer from atelectrauma, increased work of breathing or derecruitment and hypoxemia.
- T high: T high is the duration of time spent at P high and is the driving factor for the respiratory rate. The T high is often set between 4 and 5 seconds. If the T high is too short, derecruitment and hypoxemia can occur. If T high is too long, the respiratory rate will decrease leading to hypercapnia.
- P low: P low is the target pressure during the release phase. P low is generally set at zero to maximize peak expiratory flow rate. However, a P low of 0 cm H20 is never reached during expiration, if the T low is sufficiently brief, generating intrinsic PEEP to stabilize the open lung. The exhaled tidal volume is determined by the pressure gradient between the P high and P low as well as the duration of T low.
- T low: T low is the time spent at P low and is critical to control end-expiratory lung volume. T low is often initially set to 0.5 second, but should be titrated to the expiratory flow curve to prevent airway closure. It is very important to avoid setting a T low that is too long, as it will lead to alveolar collapse, causing ventilator-induced lung injury via atelectrauma from repeated opening and closing of alveoli during each tidal breath. One way to assess whether T low is too long is to examine the expiratory flow waveform. Expiratory flow should never return to the zero baseline in APRV. Instead, cycling should occur at 50% to 75% of peak expiratory flow to maintain adequate intrinsic PEEP to prevent atelectasis and derecruitment. If the static lung compliance is very poor, the T low will need to be shorter as expiratory flow is more rapid. The T low is targeted to allow ventilation but avoid derecruitment. Conversely, if the T low is too short, the volume of the release breath will not be adequate to clear CO2.
- FiO2: Fraction of inspired oxygen titrated to a target saturation of 92-96%.
References:
Owens, W. (2018). The Ventilator Book. First Draught Press, 2012.
Nieman, G., Gatto, L., Andrews, P., Satalin, J., Camporota, L., Daxon, B., Blair, S., Al-khalisy, H., Madden, M., Kollisch-Singule, M., Aiash, H., Habashi, N. (2020). Prevention and treatment of acute lung injury with time-controlled adaptive ventilation: physiologically informed modification of airway pressure release ventilation Annals of Intensive Care 10(3):1-16. https://dx.doi.org/10.1186/s13613-019-0619-3
Jain, S., Kollisch-Singule, M., Sadowitz, B., Dombert, L., Satalin, J., Andrews, P., Gatto, L., Nieman, G., Habashi, N.(2016). The 30-year evolution of airway pressure release ventilation (APRV) Intensive Care Medicine Experimental 4(11):1-18. https://dx.doi.org/10.1186/s40635-016-0085-2
Farkas, J. (April 2020). Guide to APRV for COVID. Retrieved from https://emcrit.org/ibcc/covid-aprv/
