Tracheostomy tube dislodgement
The ENT resident notifies you of an incoming tracheostomy patient who is presenting to the emergency department (ED) with difficulty breathing. The patient is a 63-year-old woman who reports having a mucus plug that she was unable to suction at home. She suffered a significant neck stabbing injury one year ago, resulting in esophageal laceration, hypoglossal nerve injuries bilaterally, and marginal mandibular nerve injury. She underwent left vocal cordotomy and supraglottoplasty 6 months ago followed by tracheostomy 5 months ago. On arrival to the ED, EMS reports they were unable to suction and the inner cannula fell out. On your assessment, she is in severe respiratory distress and her tracheostomy tube is decannulated with mild bleeding at the stoma site. She becomes increasingly agitated. The patient is moved to a room on the EMS stretcher, but you notice she suddenly becomes unresponsive. No pulses are palpable. ACLS protocols are initiated, and you are the code leader. What is your approach to the resuscitation of a tracheostomy patient in cardiac arrest secondary to hypoxemia? How will you secure the airway?
Tracheostomy tube (TT) decannulation or dislodgement is the second most common complication of tracheostomies after obstruction. Resuscitating a patient with a tracheostomy can be extremely challenging, given the risk of acute decompensation. When accidental dislodgement of a TT leads to cardiac arrest, even airway experts like ED physicians can become overwhelmed. It is important to have an organized approach to tracheostomy emergencies to stay calm in these stressful situations (Figure 1).
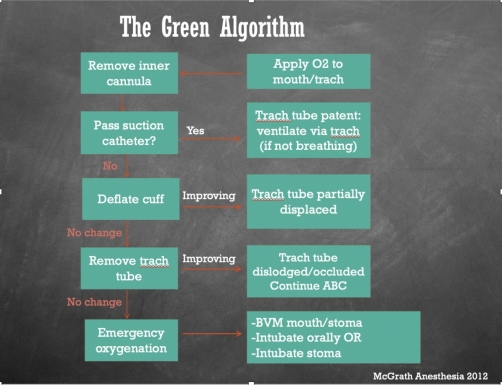
Figure 1.
- Know your tracheostomy
When managing any tracheostomy patient, especially those who are unstable or in cardiac arrest, you should know the answers to these 3 critical questions, as they have major implications for clinical management. During the code, delegate a team member to gather this information.
- When was the tracheostomy placed/how mature is the stoma? If less than 14 days, you risk creating a false track with reinsertion of a TT or ETT without fiberoptic guidance.
- Why was it placed? Was there an upper airway mass/obstruction? Was a laryngectomy performed? If so, orotracheal intubation might not be possible, and intubating through the stoma is your only option!
- What is size/type of tracheostomy tube? Cuffed or uncuffed? Size 6 or 8? What equipment do you need to replace the decannulated TT and what back up options do you need at bedside?
- Oxygenate and ventilate
The first step is to apply high-flow oxygen or support ventilation with bag-valve mask, if the patient has inadequate respiratory effort. It is important to ventilate both the mouth/nose as well as the stoma.
- Pass suction catheter
Since the tracheostomy tube is already decannulated, you can bypass removal of the inner cannula. The next step is to pass a suction catheter via the stoma as a diagnostic and therapeutic maneuver, as you continue to provide BVM support of the upper airway. If the patient improves with deep in-line suction, a mucus plug was likely present.
4. Intubation: know you airway options
If there is no change in the patient’s condition with suctioning, the next step is to intubate. It is crucial to reinsert the tracheostomy tube or perform orotracheal intubation in a timely manner, especially if hypoxic arrest is impending or has already occurred. Appropriate ventilation and oxygenation needs to be established swiftly and efficiently. If the patient’s upper airway is intact, you can proceed with standard orotracheal intubation or stoma intubation, but you must occlude the stoma after orotracheal intubation to ensure adequate ventilation. If the patient is an obligate neck breather (i.e. laryngectomy has been performed), proceed with ventilation of the stoma via pediatric LMA or facemask with a good seal over the stoma followed by stoma intubation. You can either intubate the stoma with a cuffed tracheostomy tube (with the obturator in place, followed by removal of obturator and insertion of inner cannula for ventilation) or a cuffed ETT (5.0 or 6.0). Always use a cuffed TT or ETT for patients with respiratory arrest or acute respiratory failure, to allow mechanical ventilation without a leak. Ensure that you pass the ETT just until the cuff disappears, otherwise you are at risk of mainstem intubation given the proximity of the stoma to the carina. If you have time and the right equipment, the utilization of a pre-loaded fiberoptic intubating bronchoscope is best for direct visualization.
- Know your resources.
Do not be afraid to call your ENT, interventional pulmonologist, or anesthesia colleagues (depending on where you practice) for backup or expertise. Bring in respiratory therapy as soon as possible, as they may have access to back-up TT and other equipment. Delegate a team member to gather additional back up equipment, in addition to the traditional airway essentials as below:
Equipment:
Patient's baseline size TT and one size down
5.0 or 6.0 ETT, cuffed
Lubrication for ETT or TT
Capnography
Suction
Difficult airway back-ups (bougie, cric kit, LMA, fiberoptic, etc.)
Helpful tips to remember when resuscitating the tracheostomy patient with accidental decannulation:
- Apply emergency BVM ventilation to the face and stoma, unless you are certain the patient has undergone laryngectomy, then ventilation of the stoma is sufficient.
- Always use a cuffed TT or ETT for patients with respiratory arrest or acute respiratory failure, to allow mechanical ventilation without a leak.
- Ensure adequate lubrication of ETT or TT when passing it through the stoma.
- Consider fiberoptic guidance, if the tracheostomy was placed less than 2 weeks ago.
- When inserting the TT or ETT into the stoma, tilt the patient’s head back to allow for more natural alignment of the trachea and easier insertion.
See these previous posts about tracheostomies for more reading and review of the basics!
https://emdaily.cooperhealth.org/content/tracheostomy-basics
https://emdaily.cooperhealth.org/content/tracheostomy-emergencies
https://emdaily.cooperhealth.org/content/tracheostomy-decannulation-cap-or-not-cap
References:
Long, B., & Koyfman, A. (2016). Resuscitating the tracheostomy patient in the ED. The American journal of emergency medicine, 34(6), 1148-1155.
McGrath BA, Bates L, Atkinson D, Moore JA. Multidisciplinary guidelines for the management of tracheostomy and laryngectomy emergencies. Anaesthesia. 2012;67:1025-1041.
