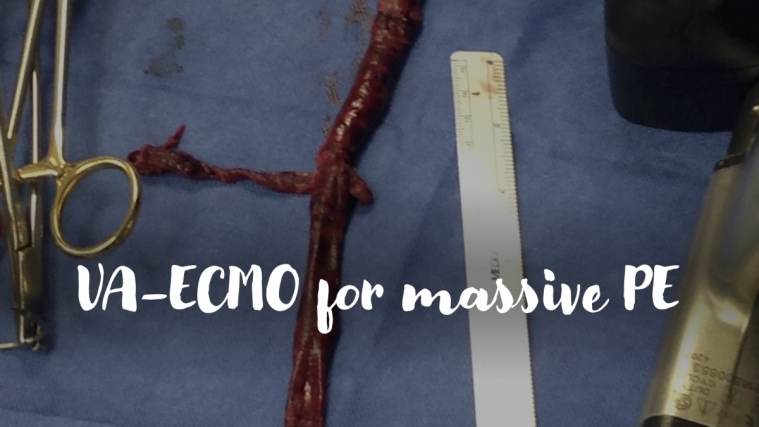
VA-ECMO for massive pulmonary embolism
A 60-year-old man presents to the ED after an episode of syncope. He is initially hemodynamically stable and undergoes CT demonstrating saddle pulmonary embolism. He returns from radiology with tachycardia and hypotension refractory to fluids and requiring vasopressor support. ECG shows sinus tachycardia with ST depression and T wave inversion in V1-V3 and the inferior leads. Bedside echo reveals right ventricular (RV) dilation and severely reduced RV systolic dysfunction with septal flattening consistent with RV pressure overload. As you start systemic anticoagulation with heparin, you consider the indications for thrombolysis, surgical embolectomy and VA-ECMO.
Systemic thrombolysis has been shown to improve mortality of patients with acute massive PE in meta-analyses as well as a small randomized controlled trial of 8 patients, although carries the risk of major bleeding. In patients with massive PE complicated by cardiac arrest or shock refractory to vasopressor and inotropic support, VA-ECMO can be considered as a bridge to surgical embolectomy or RV recovery. The goal of VA-ECMO is to maintain tissue perfusion while awaiting improvement in RV function or definitive surgical intervention. VA-ECMO decompresses the RV via venous drainage from the inferior and superior vena cava before it reaches the right heart. Survival is highest when VA-ECMO is initiated during progressive cardiogenic shock prior to cardiac arrest. Typically, concomitant systemic thrombolysis is avoided when VA-ECMO is deployed. For patients with persistent RV failure after several days of anticoagulation and mechanical circulatory support, surgical embolectomy can be performed. Conversely, if RV function improves, patients can undergo decannulation and avoid invasive surgical intervention.
Pasrija and colleagues performed a retrospective review of all patients who underwent surgical embolectomy or VA-ECMO for treatment of massive PE between 2010 and 2017 at the University of Maryland Shock Trauma Center. Patients were managed with a protocolized surgical approach using VA-ECMO as the primary intervention versus historical control group where the primary planned intervention was rapid surgical pulmonary embolectomy with use of VA-ECMO only at the discretion of the surgeon. The protocolized approach strictly followed an algorithm where all patients with normal end-organ function and intact neurologic exam went directly to the OR for embolectomy, while patients with end-organ dysfunction and unclear neurologic status were placed on VA-ECMO using a femoral venous drainage and femoral arterial return configuration. ECMO flow was titrated up until the RV was decompressed. Anticoagulation with heparin targeted a partial thromboplastin time of 72-113 seconds. Decannulation was subsequently performed for those patients with normalization of RV size and function. For patients with continued RV dysfunction, surgical pulmonary embolectomy was then performed. Patients who did not undergo surgical pulmonary embolectomy or VA-ECMO were excluded from the study (n = 3 patients).
In total, 56 patients were enrolled, including 29 patients in the protocol approach group versus 27 patients in the historical control group. All patients had severe RV dysfunction on TTE with PE confirmed by CT. CPR was required in 21 percent of all patients with no difference between the two groups. Systemic thrombolysis was performed in 21 percent of the protocol group and 15 percent in the historical control group. VA-ECMO was utilized in 93 percent of patients in the protocol group for a mean duration of ECMO support of 5.8 days. In the historical control group, VA-ECMO was used as a bridge to rapid surgical intervention in only 22 percent of patients with a median duration of 1 day. Post-op ECMO was required in 1 patient in the protocol group versus 4 patients in the historical control group. Overall, 100 percent of patients in the historical control group underwent embolectomy versus 48 percent in the protocol approach group. In-hospital survival was 97 percent in the protocol approach group versus 82 percent in the historical control group. One-year survival was 96 percent in the protocol approach and 73 percent in the historical control group.
This study demonstrates that a protocolized approach utilizing VA-ECMO as the primary intervention for acute massive PE followed by surgical embolectomy as indicated is associated with improved long-term survival as compared to salvage ECMO as a bridge to primary surgical intervention. Admittedly, mortality of patients receiving VA-ECMO for massive PE in other series is much higher, ranging from 20 percent to 60 percent; however, ECMO was often used primarily as a salvage intervention in these studies, rather than the primary intervention. Selection bias likely contributed to the increased survival observed in this study as patients with massive PE that were deemed either ineligible for cannulation or surgical intervention or those receiving salvage VA-ECMO after cardiac arrest were excluded. This study is also limited by a retrospective observational design performed in a single center experienced in VA-ECMO where complications are minimized. However, the authors do propose that the protocolized approach for management of massive PE could be employed similarly at centers with lower VA-ECMO volume. Arguably the most intriguing finding is that over half of patients in the protocolized group supported with VA-ECMO and anticoagulation only, achieved normalization of RV function obviating the need for surgical embolectomy. This highlights the resilience of the right heart in acute massive PE and the success of VA-ECMO as a bridge to RV recovery.
References
Bazan V et al. Supportive therapy: Extracorporeal Membrane Oxygenation. Crit Care Clinics 2020;36:517-529.
Jerjes-Sanchez C et al. Streptokinase and heparin versus heparin alone in massive pulmonary embolism: A randomized controlled trial. J Thrombosis and Thrombolysis 1995;2:227-229.
Pasrija C et al. Triage and optimization: A new paradigm in the treatment of massive PE. J Thor Cardiovasc Surg2018;156(2)672-681.
