Ventilator management of bronchopleural fistula

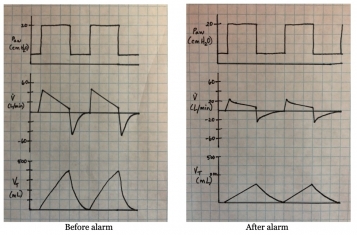
A 47-year-old man with COVID-19 pneumonia complicated by severe acute respiratory distress syndrome (ARDS) suddenly desaturates. Point-of-care ultrasound and chest x-ray are consistent with pneumothorax. After placement of a pigtail catheter, hypoxemia persists and a large continuous air leak is present. What are the next steps in management of a suspected bronchopleural fistula?