VA-ECMO for massive pulmonary embolism
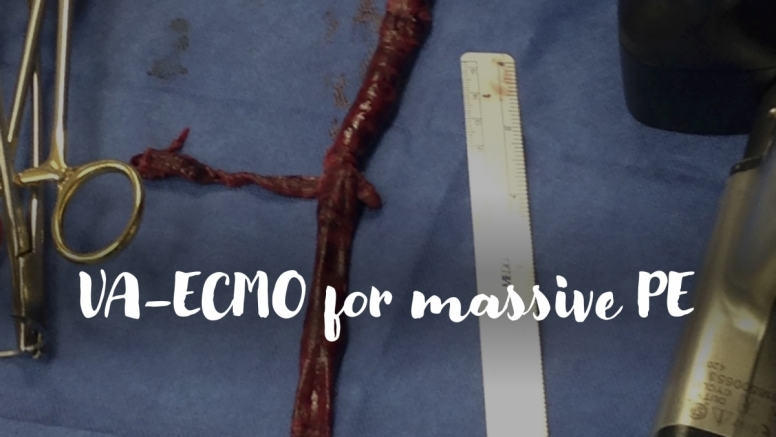
A 60-year-old man presents to the ED after an episode of syncope. He is initially hemodynamically stable and undergoes CT demonstrating saddle pulmonary embolism. He returns from radiology with tachycardia and hypotension refractory to fluids and requiring vasopressor support. Bedside echo reveals RV dilation and severely reduced RV systolic dysfunction with septal flattening consistent with RV pressure overload. As you start systemic anticoagulation with heparin, you consider the indications for thrombolysis, surgical embolectomy and VA-ECMO.